I remember exactly where I was when my cell phone rang. “It’s cancer,” said the deep voice I knew and loved so well. “Oh, hon,” I said, letting my breath out, my brain firing in all directions like that little silver ball in a pinball machine.
Photo by Sydney Rae on Unsplash
“What can we do in addition to what you’re prescribing?” we asked the medical professionals.
My husband, Gary, and I knew we didn’t want to sit around hoping surgery or treatment was all he needed; we instinctively wanted to be proactive in facing down cancer.
As time passed, we determined a plan. And it served us well.
In Gary’s case, men with late-stage prostate cancer who were relatively young and in good shape could expect to live an average of two years. But Gary was never one to accept ‘average.’
And so we recruited a team to help us live proactively. As it turned out, Gary survived ten years with late-stage disease, and most of those years were a good quality of life.
Keeping in mind that every cancer patient is unique, here are 9 signs you might be a proactive cancer patient:
1. Read … but don’t believe everything you read.
Gary and I know cancer patients who paid thousands of dollars for treatment in foreign places, who forewent treatment because they’d read supplements and a positive outlook could heal their cancer, who invested in expensive concoctions that were guaranteed to cure. None of these things panned out for our friends.
We did our share of reading—which was overwhelming because there is so much conflicting information—and we came open-minded to consultations with the medical professionals.
Eventually we set aside our reading and start living while Gary still had life.
2. Prepare for appointments.
There are some practical things we can do to be better prepared for medical consultations:
What you think to ask while at home can easily slip your mind at appointments. Write your questions down, and bring your list to consultations.
Recruit a friend or family member to attend medical consultations — preferably someone who can take good notes because it’s easy to forget important points.
Be open and honest about health history and physical quirks. We certainly don’t know more than the doctors, but we know our own bodies well. (One of my physical quirks: I get light-headed and nauseated when a prolonged ‘needle-through-skin’ procedure is taking place, even if I feel no pain. It’s because I think too much.)
3. Eat better.
I thought I fed my family healthfully — made-from-scratch meals, home-baked breads, no junk food or sugary beverages. But I baked with white flour and white sugar, and we ate white rice. So there was room for improvement.
Gary and I steered toward a plant-rich diet: We incorporated more veggies, fruits, whole grains, and legumes; eliminated unhealthful fats and sugars; and cut way back on red meats, eating small portions of poultry, seafood, and wild game instead.
Looking back, Gary’s cooperation was crucial. If he had resisted me on this nutritional endeavor, for the sake of keeping the peace I would have given up.
4. Get moving.
Every cancer patient is at a different level of health before the diagnosis. In Gary’s case, because he felt relatively well and because his treatment caused osteoporosis, we started pounding the pavement to strengthen bones. We eventually took up hiking and snowshoeing in the nearby Cascade Mountains.
For others, more movement might simply mean a gentle walk around the block.
Gary and I didn’t think changing our diet and exercising more was going to cure his cancer. But along with extended life, we were also shooting for quality of life. And eating better and adding more movement certainly helped achieve that goal.
Disclaimer: Before you make any changes to diet or physical activity levels, first consult with your physician.
5. Manage the stress.
Whether we’re the patient or the caregiver, cancer comes with a considerable amount of stress.
Gary and I discovered some rather inexpensive, fun things that helped us manage the stress:
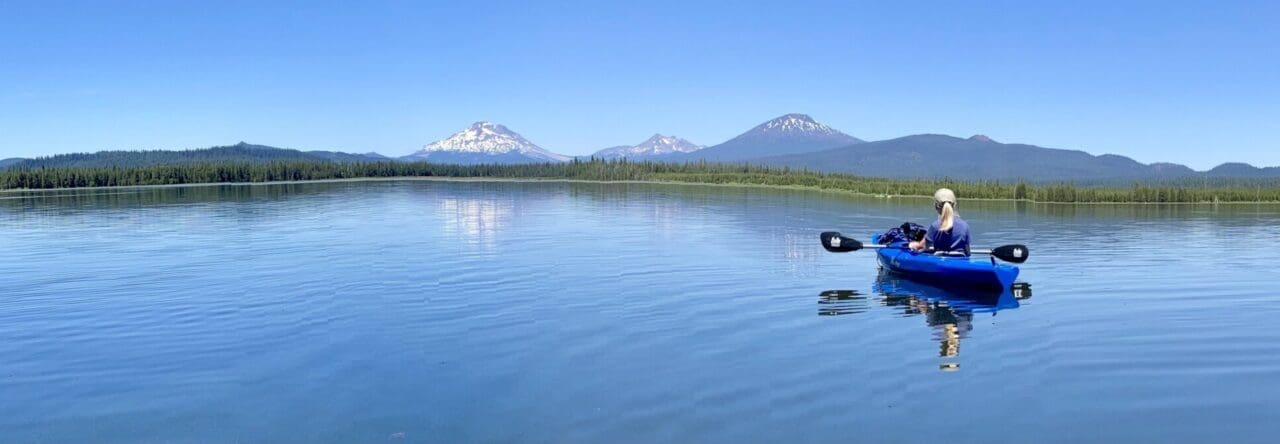
Getting outdoors was a big one — whether hiking to the top of a mountain, or sitting in lawn chairs in the park as geese announced their take-offs and landings on the river.
We established a standing Friday date, which almost always included a hike followed by some great food.
We enjoyed good books and movies, and enjoyed discussing them afterward.
We practiced living in the present, paying attention and counting all that remained instead of all that would never be the same.
For pain and stress management, ask your oncologist about oncology massage, lymphedema massage, or acupuncture.
6. Get connected.
Joining a group of people who have experienced what we’re going through—whether the group is sitting in a circle discussing the ramifications of being a cancer patient or caregiver, or they’re doing an activity together—can nourish strength and hope. Powerful words, these: “I get it”, “I’ve been there”, and “Here’s what helped me.”
7. Practice gratitude.
Gary and I weren’t grateful for cancer interrupting our lives, bullying us, arriving at a time when our finances were fragile due to a job lay-off.
But in time, we learned to count all the things that made up a gleeful and brimming life:
- Kids and grands who think the world of us
- Relentless, energetic, generous friends and extended family
- Roof over our heads, cupboards stocked with food, switches that magically turn on lights and heat
- FaceTime conversation with all six grandkids at once — zaniness!
- Aroma of cinnamon candle flickering
- Beauty of snow tumbling every which way
- One more day with my beloved
8. Give back.
Finding a way to give back can add meaning to an otherwise senseless diagnosis. Gary and I established a non-profit and, working around our day jobs, traveled across the country presenting what we were doing to live well with terminal disease.
One of my cancer survivor friends knits prayer shawls for chemo patients, and another friend who is a cancer caregiver rocks frail newborns in the NICU at the local hospital.
Giving back takes our thoughts off our own losses as we focus on the hurts and sorrows of others around us.
9. Consider hospice care for the terminal patient.
When Gary opted out of a last chemo possibility, the oncologist suggested a referral for hospice care.
I remember thinking: Wait … what? Isn’t it too soon?!
Most people think hospice care is for the last few weeks and days of life. But it’s not. It’s for the terminal patient who decides to forego additional treatment or surgery. The hospice team’s goal is to provide care in the comfort of the terminal patient’s home. And it’s better to get them onboard before there is a crisis.
::
Even though Gary and I didn’t fully understand the value of being a proactive patient and caregiver, it was one of the wisest things we did.
Because proactivity says, I’m not sitting back, hoping surgery or treatment is all I need.
It says, I’m going to live a brimming, fierce, courageous life — as much as it depends upon me.
Take that, cancer.
P.S. If you know of someone who needs to be encouraged toward proactivity, please share, tweet or pin!
Melinda Poling
Thank you Marlys, for this! So practical and touching.
Marlys Johnson
It seems that so much of handling adversity well comes down to the practical, doesn’t it, Melinda? Like, making healthful choices, learning to lean on the strength of others, adjusting our attitudes. And for those of us who are believers in Jesus Christ, there’s the added grace of knowing we’re held in the hands of the Creator of the universe, that this hard thing isn’t some random event that caught God by surprise. Thank you for your comment!