My friend, upon turning 40, had a mammogram. Suspicious areas showed up in both breasts, which precipitated an ultrasound, two biopsies and additional mammography. All to the tune of $4,000. Although no cancer was detected, my friend needs to return every six months for images. “High risk,” they said. “We need to watch this closely,” they said.
Here’s the catch: Her insurance pays for preventive mammography, but not diagnostic mammography. Which means the ongoing imaging will be a significant out-of-pocket expense.
Short of propping open a guitar case and strumming on the streets, what’s a person to do?

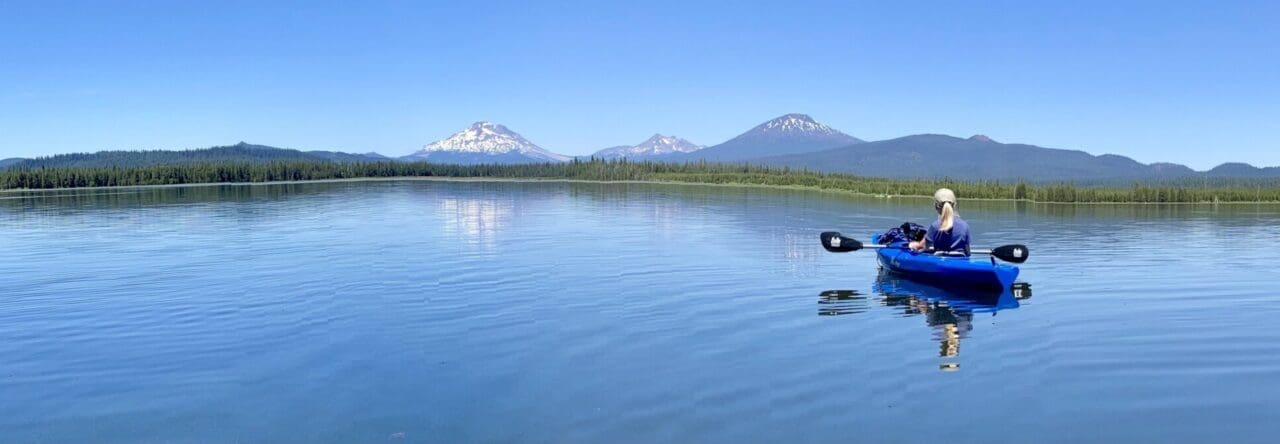
Photo credit: Pixabay
In our case, Hubby and I had healthcare coverage, but were coming off a two-year unemployment period and had already gone through the anguish of selling our home and cashing out our retirement investments to stay afloat. And then those fearsome vexatious daunting words: “You have cancer.”
Which begs the question: Does the stress of financial issues hinder the healing process for the cancer patient?
The answer, unfortunately, is yes.
In fact, there’s a term for it: financial toxicity. Scott D. Ramsey and Veena Shankaran write about financial toxicity as being the “other” toxic side effect of cancer treatment.
This from Christopher Lathan, MD, and lead author of a study published by researchers at the Dana-Farber Cancer Institute:
We found that patients who had financial distress at the time of diagnosis were more likely to have poorer outcomes in physical and mental quality of life measures, pain, and symptom burden.
With that in mind, here are 6 suggested tactics to help in the area of financial toxicity:
Ask your medical team for recommendations.
Patient advocates, oncology social workers, case managers, doctors and oncology nurses — those who are in the trenches alongside the patients — can be a wealth of information regarding support services. Don’t be hesitant to say: “This is all new to me; I’m going to need some financial help; where do I begin?”
Inquire into pharmaceutical drug assistance programs.
Most pharmaceuticals run programs to assist patients who are in financial difficulties and are not eligible for Medicare, Medicaid, or private insurance. Ask your doctor if you qualify for pharmaceutical drug assistance (programs require the physician to register the patient).
Check out national financial support resources.
A list of resources is posted at Cancer.Net under the heading “Financial Resources.” The list includes national service organizations; housing and travel assistance programs; assistance with medication and treatment costs; and general financial information. Although this list is robust, it isn’t exhaustive.
Look into local financial support resources.
You might be surprised at the number of people in your community who have been adversely affected by cancer and, as a result, established some sort of venture to assist cancer patients and their families. In 2008, I self-published a book featuring a number of cancer survivors and caregivers from across the country who chose to give back in practical ways, mostly within their own communities.
Here are four people/families featured in the book:
16-year-old Jan-Willem. Jan-Willem Knapen had the idea for a house on hospital grounds that would provide families and individuals rest and self-care while their loved ones were in the hospital. Although dealing with brain cancer, JW began raising funds for the house. After he died, his family and the community banded together to see his dream come to fruition, and the doors of JW House (Santa Clara, CA) opened in 2008.
Kelly Turner, New Haven, CT, police officer. The C.H.A.I.N. Fund, Inc. was founded by Kelly Turner after police officers and firefighters banded together with financial support to see Kelly through her long recovery from breast cancer and surgery complications. The C.H.A.I.N. Fund provides a variety of financial and support services to people whose lives have been altered by cancer and who wouldn’t otherwise qualify for government assistance.
Brown University student Doug Ulman. The Ulman Cancer Fund for Young Adults was founded by Doug Ulman and his family after he was diagnosed three times with cancer during his years as a student at Brown University. The Ulman Fund offers one-on-one support, meet-up groups, education, household assistance and scholarships for young adults with cancer.
Richard and Diane Nares, parents of 5-year-old Emilio. After Emilio Nares died of acute lymphoblastic leukemia, his parents, Richard and Diane, created the Emilio Nares Foundation (now serving three counties in southern California) to help low-income families meet basic needs: transportation to and from cancer-related appointments; assistance with groceries, electric bills, and finding homes for displaced families; and a resource center with trained bilingual staff members to help families understand information on cancer, treatment, housing, employment, and financial and legal aid.
Inquire about payment options.
A number of medical centers and clinics will negotiate with the patient and/or help set up a doable payment plan. Try to meet in person with the billing department. State your case, letting them know you want to make payments, and ask if they can give you a break on the rates and set up a payment plan. It costs nothing to ask.
Accept a friend’s offer to organize a crowdfunding effort.
There are a number of crowdfunding platforms that allow a family member or friend to create a website to collect donations and post patient updates. These platforms—GoFundMe, GiveForward, Fundly, Kickstarter and others—keep 5-10% of funds raised.
A friend recently suggested an alternative, YouCaring, that charges no fee, which means 100% of the donations go directly to the cause. “I have friends with family members who are cancer patients who have used it with great success,” wrote my friend.
* * *
Although these six tactics don’t come anywhere near solving the country’s challenges over healthcare costs, I love the big-heartedness, dignity, resilience, far-reachingness of people who have faced adversity and then decided to become proactive in giving back to others on a similar journey.
What other ideas or tactics have you heard about or experienced firsthand for handling financial toxicity?
P.S. If you found this post encouraging or informational, please share, tweet or pin!
Karen Henderson
When I had my 1st Pacemaker /Defibrillator I had just had several very expensive tests, heart procedures and hospital stays. I still had not reached my Annual Deductible yet for the year. The Pacemaker /Defibrillator was at that time about $100,000 for the unit, Cardiologist Surgeon, hospital….. We lived in a town at that time that had 2 hospitals not owned by the same large Company. My Doctor told me to contact the Hospital that my insurance required me to use & then get a quote for the portion of the bill I would be required to pay. Then I was to call his Secretary and tell her the amount. She called the other Hospital and gave them all the information. They NEGOTIATED and accepted the amount my insurance was willing to pay them, which I assume was 80%. My part was 0.
Marlys Johnson
That’s awesome, Karen. What a great example. Thanks for sharing!